Oocyte
Maternal obesity, oocyte health and pregnancy outcomes
Mitochondrial DNA and oocyte competence
Recent studies have evaluated mitochondria (mt) and its maternally-inherited genetic material, mtDNA, in oocyte function and its potential role in fertility. Mitochondria are organelles involved in energy production and the programmed cell death pathway, apoptosis, in cells such as oocytes. These functions make mitochondria integral to oocyte function and subsequent embryo development. Mitochondrial dysfunction has been linked to decreased fertility as well as to developmental retardation of the embryo. As women age, mitochondrial activity decreases; this process is thought to contribute to declining fertility and lower pregnancy rates in older women compared to younger women. Although the mechanism behind declining mitochondrial activity with advanced maternal age is unclear, one group has shown that an accumulation of mutations in mtDNA in oocytes over time could ultimately lead to decreased implantation rates and increased rates of genetic abnormalities such as aneuploidy seen at an increased rate in older women compared to younger women.
Recent research has investigated the role of mtDNA on fertility. Wai et. a/. found that embryos with the highest likelihood of successful development are those with the greatest mtDNA content; mitochondrial copy number in oocytes is directly related to fertility. Older women (>35 years of age), however, have decreased mtDNA copy number in oocytes and poorer ovarian response compared with younger women. Older women also have greater mtDNA mutations detected in blood samples, as evidenced by the common mutation 4977 bp in mtDNA [8]. This group also found that an increased incidence of mtDNA mutations such as the mutation they specifically evaluated as well as decreased mtDNA copy number in older woman may reflect ovarian aging. Although these findings elucidated the role of mitochondria in fertility, little is known about the specific mutations and the level of heteroplasmy in mtDNA detected at the level of each oocyte. Our goal in this project is to identify heteroplasmic mtDNA mutations at the level of a single human oocyte that can lead to decreased IVF efficiency and fertility.
Sperm
Paternal environmental exposures and reproductive outcomes
To date, there are limited data to explain the underlying mechanisms whereby paternal environmental exposures result in adverse reproductive events. These potential paternal exposures are reported predominantly within occupational, industrial, and military settings and a priority list of hazardous substances exists within section 204 of the Comprehensive Environmental Response, Compensation, and Liability Act. Based upon the frequency, toxicity, and potential for human exposure Benzo(a)pyrene (BaP) and polyaromatic hydrocarbons (PAHs) fall within the top ten on this list. PAHs, represent a class of highly toxic and widely dispersed environmental hazards which are formed as the unintentional byproducts of industrial processes such as incineration, burning treated wood, the incomplete combustion of fossil fuels, and diesel truck exhaust which may then be absorbed as particulate matter. PAHs bind with high specificity and affinity to the aryl hydrocarbon receptor (AHR, AHR, Ahr) which is essential to xenobiotic metabolism and important physiologic processes such as cell growth, death, and differentiation.
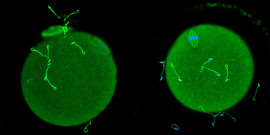
We have established a unique toxin informed laser microdissection (LMD)/qRT PCR assay using cigarette smoke condensate (CSC) to detect changes in gene expression in distinct sperm cell populations consistent with AHR activation and oxidative stress. Our data suggests that spermatocytes are vulnerable to environmental insult via AHR pathways. Our lab is the first to localize AHR to the sperm flagellum and the acrosome which is consistent with AHR physiologic functions, its role in xenobiotic metabolism, the exposure of post testicular sperm to toxins via seminal fluid, and the need to respond to oxidative stress. Our data suggests that AHR dysregulation may impact the energy, structure, and motility necessary for fertilization. Finally, we observed male reproductive tract abnormalities in the AHR knockout male (Taconic Farms 9166M) to describe: a) increased apoptosis of spermatocytes; b) reduced sperm count and decreased motility; c) atypical sperm morphology characterized by a blunted acrosome, distorted connecting piece, and abnormal flagella; and d) decreased fertilization. It is our hypothesis that AHR loss of function will inform AHR gain of function in toxin exposed males.
Insulin rescues impaired spermatogenesis via the hypothalamic-pituitary gonadal axis in Akita diabetic mice and restores male fertility
The mechanism responsible for poor reproductive outcomes in male diabetics is not well understood. In light of new evidence that the Sertoli cells of the testis secrete insulin, it is currently unclear whether diabetic subfertility is due to deficiency of pancreatic or testicular insulin or both. The Akita mouse diabetic model, which expresses a mutant, non functional form of ins2 in testes and pancreas, was used to determine the implications of systemic vs local effects of insulin deficiency on the process of spermatogenesis and fertility. We have found that Akita homozygous male mice are infertile, have reduced testis size and abnormal morphology. Spermatogonial germ cells are still present, but are unable to differentiate into spermatocytes and spermatids. Exogenous insulin treatment regenerates testes and restores fertility, but this plasma insulin cannot pass through the blood testis barrier. We conclude that insulin does not rescue fertility through direct interaction with the testis, but instead by restoring function of the hypothalamic pituitary gonadal axis thus normalizing hormone levels of LH and testosterone. Although we show that the Sertoli cells of the testis secrete insulin protein, this insulin does not appear to be critical for fertility. Our current studies are exploring leptin and its ability to rescue the male infertility phenotype.